Consider This Important Evidence First When Thinking About Using Vaginal Dilators:
Retraining the Body’s Response to Penetration with Mindfulness Approaches to Genito-Pelvic Pain/Penetration Disorder

Imagine being able to help your clients suffering from Genito-Pelvic Pain/Penetration Disorder (GPP/PD) with a treatment that not only addresses physical discomfort but also the emotional and psychological toll of this vaginal condition.
Such treatment exists and it’s known as somatic emotional awareness, or mindfulness, in the treatment of GPP/PD. Today, let’s explore the benefits of incorporating mindfulness into the rehabilitation process for your clients which vaginal dilator therapy is indicated for.
Considering A Mindfulness Approach To Treating GPP/PD
Have you seen the evolving literature indicating the use of psychotherapeutic approaches (including mindfulness and cognitive behavioral therapy (CBT)) for treating GPP/PD? Would you be surprised to learn the approaches are implemented and successful with or without vaginal dilator therapy?
Any seasoned pelvic health therapist knows a mindfulness approach is helpful in treating GPP/PD in conjunction with dilators, but what if you took it a step further and used mindfulness training with your clients before ever even discussing dilators?
By the end of this article you’ll have more tools to better help your GPP/PD clients and be able to change your treatment approach in the clinic as soon as tomorrow!
Does This GPP/PD client Sound Familiar?

Many women respond well to dilator intervention with no mindfulness application. Women who are recently postpartum, normally enjoy sex, but experience pain during it, and who want to get back to sexual activity, are likely to respond well to dilator therapy, and they often do quickly.
Other times, women like Jill will walk into your clinic. Jill has had GPP/PD for seven years, and she experiences pain and immense anxiety every time she attempts to have penetrative sex. Jill’s goals are to have vaginal penetration without pain, and to enjoy the experience.
Jill brought her condition up to her primary care provider in the past and was told to drink wine, take Valium, and “just relax”.
When presented with the idea of using a dilator, Jill is excited at the prospect of a treatment that could help her, but feels there is no way she can insert a dilator.
Clearly, jumping straight to a dilator approach won’t be the most efficient or appropriate route for Jill. Instead, you decide to address her GPP/PD with a mindfulness approach first.
You may not attempt any internal examination for several visits. You may not even bring out any wands or dilators, or talk about “stretching” her vagina, either. Jill may need to start with visualization exercises instead of the traditional route.
Jill may respond well, and see symptom improvements in just a few weeks using consistent mindfulness practices.
Once she’s comfortable, Jill can progress to dilator therapy. Starting with dilators right from the beginning, Jill is the type of client who would have likely stopped coming to her visits, or worse, had an exacerbation of her condition.
These clients are so happy to finally be able to take control of their condition and have a selection of tools to use as they continue to progress.
Traditional Approaches to Treating GPP/PD: Vaginal Dilators Alone

Historically, the go-to recommendation for improving vaginismus or GPP/PD often involves the use of a vaginal dilator. However, considering dilator use as the only course of care for GPP/PD means attending only to the musculoskeletal system while ignoring how the somatic-emotional context translates to a person’s arousal and sexual activity.
The approach to using a dilator to “stretch” muscles for the sole outcome of penetration may be inappropriate and even detrimental to some clients’ progress.
Your clients may experience:
- Inability to have a pelvic examination or be sexually active with vaginal penetration
- Anxiety surrounding thoughts and sensations that arise from using dilators
- Re-traumatization and exacerbation of symptoms with thoughts of using a dilator
The lack of a mindful approach to using vaginal dilators disregards the importance of connecting with one’s own body and creating space for a positive experience.
If you choose to try a dilator with a client, introduce it as a tool not to achieve penetration, but as an option that your client can “invite” or “accommodate” into their physical and emotional experience. Adding mindfulness practices to your approach can help make the process of treating GPP/PD less overwhelming and more empowering for your clients.
Exploring Causes of GPP/PD

It is important to consider that overactive pelvic floor musculature (PFM) has many causes including both somatic and emotional components. Many cases of GPP/PD may involve clients who did not have good access to sexual education, or who have been exposed to negative, shameful, or fearful attitudes about sex and sexuality.
Others may not have had experience or permission to explore what their own bodies enjoy regarding touch, pleasure and arousal. Medical, emotional, and physical traumas are often also present, and many of these conditions exist at the same time.
Because of this, each client requires a holistic and individualized approach. Consider incorporating mindfulness and somatic emotional components within each plan of care.
What Is Mindfulness, Anyway?
Mindfulness is considered a mental state achieved by purposefully focusing one’s awareness on the present moment, while calmly acknowledging and accepting one’s feelings, thoughts, and bodily sensations as each successive moment continuously unfolds.
Mindfulness is a form of intentional and non-judgmental awareness that allows individuals to gain insight into their own thoughts and emotions, and to experience a greater sense of well-being.

By paying attention to the present moment, individuals can develop a greater sense of self-awareness and a more positive relationship with themselves and the world around them. Generally, practicing mindfulness can reduce stress, increase emotional regulation, and improve physical and mental health. It can be practiced through various techniques with or without professional guidance.
Applying this phenomenon to your clients, you can see how impactful a mindfulness approach can be for someone struggling with GPP/PD, especially when a history of trauma, shame, or guilt are involved.
Why You Should Consider Incorporating Mindfulness When Treating GPP/PD
Research shows a strong link between GPP/PD and anxiety, distress, and specific phobias related to sexual activity. Research also indicates the involuntary tightness of the pelvic floor with any kind of touch or penetration may be associated with the defense reaction of the body in response to perceived stress.
Rather than viewing this as a dysfunctional response, it is important to understand the body is actually trying to protect itself from potential harm (McEvoy, 2021). With persistence, patience, and biopsychosocial support, the body can learn to perceive genital self exploration or sexual encounters as non-threatening and enjoyable experiences.
Incorporating mindfulness practices into the treatment of GPP/PD can not only enhance the rehabilitative experience, but can lead to improved outcomes for your clients as well.
Can Mindfulness Serve As An Alternative To Vaginal Dilators?

Emphasizing the importance of mindfulness and developing increased body awareness can help individuals become more in tune with their physical sensations, thoughts, reactions, and emotions associated with GPP/PD.
By creating a positive experience and fostering a greater sense of body awareness, individuals are more likely to feel empowered and motivated to understand what they find pleasing or discomforting in relation to arousal and penetration.
Mindfulness may allow for clients to feel more relaxed, centered, and in control, which can be particularly helpful in reducing anxiety or stress associated with GPP/PD.
Darnell (2021) presents a model demonstrating how a client can gradually progress body exploration while tracking how the body communicates feelings and emotions and paying attention to where these feelings and emotions are felt in the body as they emerge.
Building a foundation of mindfulness prior to initiating dilator training will likely set your client up for both physical and emotional success along their healing journey.
As you can see, this approach may be a good alternative to simply focusing on dilators as a first line of treatment.
Emerging Evidence Supports the Use of Mindfulness in Treating GPP/PD

In 2022 Pernilla showed that attentional focus influences the sexual response, and mindfulness skills have been linked with an enhanced ability to purposefully direct attention to and generate awareness of bodily sensations. Mindfulness-based approaches have also been associated with improved somatic and emotional regulation.
For example, if sexual interactions trigger thoughts of self-criticism or anxiety, approaching these emotions in an open and non-judgmental way may reduce the emotional impact on the client’s sexual experience.
In another study (Silverstein et al, 2011) demonstrated that following participation in a mindfulness course, subjects reported reduced levels of self-judgment, reduced symptoms of anxiety and depression, and an increased awareness of their sexual response — further supporting the use of mindfulness in treating GPP/PD.
It’s clear that incorporating mindfulness into the process of treating GPP/PD can help your clients overcome negative associations or traumatic experiences which may be augmented with the use of vaginal dilators.
This approach is also helpful for those who have undergone pelvic surgery, radiation therapy, and those with other pelvic pain conditions such as vulvodynia.
Exploration Of Mindfulness Techniques In The Treatment Of GPP/PD
Darnell (2021) presents the use of mindfulness in clinical practice within the notions of interoception (observing the body and monitoring the sensations within) and exteroception (extending observation to the surrounding environment).
Here are three examples of interoceptive mindfulness practices for clients with GPP/PD:
- Mindful meditation: This can be done through guided meditations, deep breathing exercises, or simply taking a few moments each day to focus on the present moment and bring awareness to thoughts, feelings, and physical sensations.
- Self-reflection: Your client may find it helpful to take time each day to reflect on the day’s thoughts and feelings, without judgment. This can help increase self-awareness and emotional regulation. Using a journal is an easy way to track and report progress.
- Connecting with the body: Engage in activities that improve the likelihood of someone feeling more connected to their body, such as yoga or exercise. This practice of regularly being present “in the body” can be beneficial for your clients.

There are several strategies for a client to bring their body from a state of heightened tension to a state of relaxation and resilience. Other tools may include breath work, or exteroceptive practices such as aromatherapy, and light therapy.
What works for one client in one session may not work the next time, or for the next client. Having a variety of tools in your toolbox will better prepare you and your clients to navigate this process in a more meaningful way.
In order to best suit your client’s present needs, it may be helpful to first query them and see if they’re already aware of specific mindful practices they’ve found helpful in the past. You can also suggest they trial a variety of techniques to discover what is most relevant for your client at any given time.
Explaining the “Why” Behind Mindfulness and Dilator Use to Your Clients
As a pelvic health therapist, you play an important role in educating your clients about the use of mindfulness in conjunction with, or prior to, vaginal dilator therapy.
To review, here are four reasons to consider educating your clients about the importance of mindfulness practices as part of your treatment plan for GPP/PD:
- Improved outcomes: By incorporating mindfulness into the process of using vaginal dilators, clients are more likely to experience less discomfort and anxiety. Addressing the mindfulness components of your client’s care can also help them become more in tune with their bodies, leading to a greater sense of self-awareness and control, which in turn increases the likelihood of recovery.
- Increasing compliance: By educating clients about the benefits of mindfulness practices in conjunction with their rehab, you can help increase client compliance and motivation to continue to progress to or through using vaginal dilators. Better compliance and consistency with their plan of care can ultimately lead to better outcomes for clients as well.
- Reducing negative associations: For clients who have experienced physical trauma or negative associations with arousal or contact with the vulva, incorporating mindfulness can help reduce these negative associations. This in turn, may decrease tissue tension, resulting in less pain and improved functional outcomes.
- Promoting client empowerment: Mindfulness can help people feel more empowered and in control of their bodies, which is particularly important for those experiencing GPP/PD
It’s important that you educate your clients about the benefits of incorporating mindfulness into the process of using vaginal dilators, whether the mindfulness is introduced before or during dilator therapy. This can help improve client outcomes, increase client compliance, and promote client empowerment.
If you treat clients who have experienced negative responses to introducing dilators, now you’ve got contextual background knowledge plus some techniques to help you take a holistic and more mindful approach to treating GPP/PD and vaginismus.
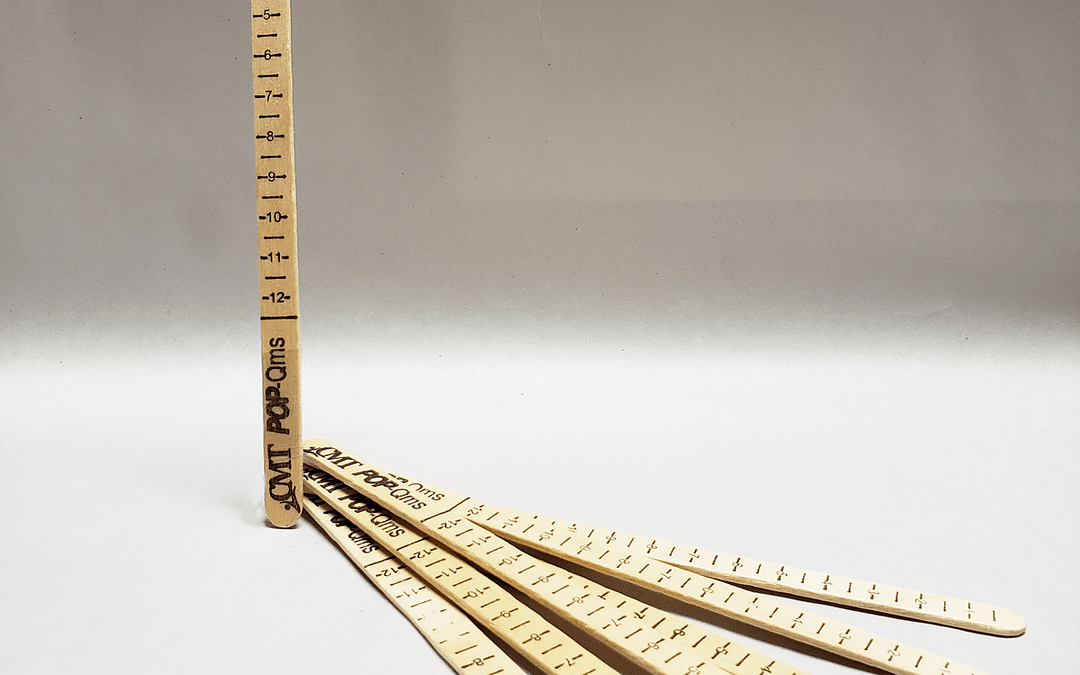
If you are looking to expand your mindfulness toolbox, I’m updating my Patient and Practitioner Handouts for Using Vaginal Dilators. These handouts are complete with done-for-you explanations of breathing techniques, preparatory activities and several different vaginal dilator techniques. Join my waitlist to be notified of product availability.
Be sure to review and share my free literature summary for more information and a deep dive into the most current research on mindfulness approaches to GPP/PD.
So, now that you’re familiarized with alternative approaches to treating GPP/PD — which client’s life will you change first?
A special thank you to Dr. Serena Fiacco, DPT, DHS, ACS from The Pelvic Health Clinic, Diane Hetrick, PT, and Eugenia Chui, SPT for providing suggestions for this blog post and valuable input on mindfulness.
Resources
Free Literature Summary – Somatic Emotional Awareness in the Treatment of Genito-Pelvic Pain/Penetration Disorders
Client and Practitioner Handouts Product Announcement – Vaginal Dilator Techniques: Educational Handouts for Practitioners and Their Patients
Darnell, C. (2021). Tending to painful sex: Applying the neuroscience of trauma and anxiety using mindfulness and somatic embodiment in working with genito-pelvic pain and penetration disorders. Sexual and Relationship Therapy, 1–13.
McEvoy, M., McElvaney, R., & Glover, R. (2021). Understanding vaginismus: a biopsychosocial perspective. Sexual and Relationship Therapy, 1-22.
Pernilla M, Lance MC, Johanna E, Thomas P, JoAnne D. Women, painful sex, and mindfulness. Mindfulness. 2022;13(4):917-927. doi:10.1007/s12671-022-01843-5
Silverstein, R. G., Brown, A.-C.H., Roth, H. D., & Britton, W. B. (2011). Effects of mindfulness training on body awareness to sexual stimuli: Implications for female sexual dysfunction. Psychosomatic Medicine, 73(9), 817–825.



Thank you Kathy for putting together the research and the application of mindfulness with pelvic pain and dilator use. That approach is critical for helping patients tune into the deepest responses and connection with their body and mind and leads to more choice and self awareness.